Comfortably seated in the fertility clinic with Vivaldi playing softly in the background, you and your partner are brought coffee and a folder. Inside the folder is an embryo menu. Each embryo has a description, something like this:
Embryo 78 – male
No serious early onset diseases, but a carrier for phenylketonuria (a metabolic malfunction that can cause behavioural and mental disorders. Carriers just have one copy of the gene, so don’t get the condition themselves).
Higher than average risk of type 2 diabetes and colon cancer.
Lower than average risk of asthma and autism.
Dark eyes, light brown hair, male pattern baldness.
40% chance of coming in the top half in SAT tests.
There are 200 of these embryos to choose from, all made by in vitro fertilisation (IVF) from you and your partner’s eggs and sperm. So, over to you. Which will you choose?
If there’s any kind of future for “designer babies”, it might look something like this. It’s a long way from the image conjured up when artificial conception, and perhaps even artificial gestation, were first mooted as a serious scientific possibility. Inspired by predictions about the future of reproductive technology by the biologists JBS Haldane and Julian Huxley in the 1920s, Huxley’s brother Aldous wrote a satirical novel about it.
That book was, of course, Brave New World, published in 1932. Set in the year 2540, it describes a society whose population is grown in vats in an impersonal central hatchery, graded into five tiers of different intelligence by chemical treatment of the embryos. There are no parents as such – families are considered obscene. Instead, the gestating fetuses and babies are tended by workers in white overalls, “their hands gloved with a pale corpse‑coloured rubber”, under white, dead lights.
Brave New World has become the inevitable reference point for all media discussion of new advances in reproductive technology. Whether it’s Newsweek reporting in 1978 on the birth of Louise Brown, the first “test-tube baby” (the inaccurate phrase speaks volumes) as a “cry round the brave new world”, or the New York Times announcing “The brave new world of three-parent IVF” in 2014, the message is that we are heading towards Huxley’s hatchery with its racks of tailor-made babies in their “numbered test tubes”.
The spectre of a harsh, impersonal and authoritarian dystopia always looms in these discussions of reproductive control and selection. Novelist Kazuo Ishiguro, whose 2005 novel, Never Let Me Go, described children produced and reared as organ donors, last month warned that thanks to advances in gene editing, “we’re coming close to the point where we can, objectively in some sense, create people who are superior to others”.
But the prospect of genetic portraits of IVF embryos paints a rather different picture. If it happens at all, the aim will be not to engineer societies but to attract consumers. Should we allow that? Even if we do, would a list of dozens or even hundreds of embryos with diverse yet sketchy genetic endowments be of any use to anyone?
The shadow of Frankenstein’s monster haunted the fraught discussion of IVF in the 1970s and 80s, and the misleading term “three-parent baby” to refer to embryos made by the technique of mitochondrial transfer – moving healthy versions of the energy-generating cell compartments called mitochondria from a donor cell to an egg with faulty, potentially fatal versions – insinuates that there must be something “unnatural” about the procedure.
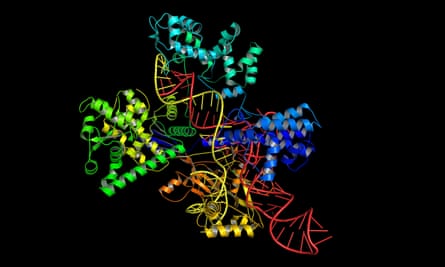
Every new advance puts a fresh spark of life into Huxley’s monstrous vision. Ishiguro’s dire forecast was spurred by the gene-editing method called Crispr-Cas9, developed in 2012, which uses natural enzymes to target and snip genes with pinpoint accuracy. Thanks to Crispr-Cas9, it seems likely that gene therapies – eliminating mutant genes that cause some severe, mostly very rare diseases – might finally bear fruit, if they can be shown to be safe for human use. Clinical trials are now under way.
But modified babies? Crispr-Cas9 has already been used to genetically modify (nonviable) human embryos in China, to see if it is possible in principle – the results were mixed. And Kathy Niakan of the Francis Crick Institute in the UK has been granted a licence by the Human Fertilisation and Embryology Authority (HFEA) to use Crispr-Cas9 on embryos a few days old to find out more about problems in these early stages of development that can lead to miscarriage and other reproductive problems.
Most countries have not yet legislated on genetic modification in human reproduction, but of those that have, all have banned it. The idea of using Crispr-Cas9 for human reproduction is largely rejected in principle by the medical research community. A team of scientists warned in Nature less than two years ago that genetic manipulation of the germ line (sperm and egg cells) by methods like Crispr-Cas9, even if focused initially on improving health, “could start us down a path towards non-therapeutic genetic enhancement”.
Besides, there seems to be little need for gene editing in reproduction. It would be a difficult, expensive and uncertain way to achieve what can mostly be achieved already in other ways, particularly by just selecting an embryo that has or lacks the gene in question. “Almost everything you can accomplish by gene editing, you can accomplish by embryo selection,” says bioethicist Henry Greely of Stanford University in California.
Because of unknown health risks and widespread public distrust of gene editing, bioethicist Ronald Green of Dartmouth College in New Hampshire says he does not foresee widespread use of Crispr-Cas9 in the next two decades, even for the prevention of genetic disease, let alone for designer babies. However, Green does see gene editing appearing on the menu eventually, and perhaps not just for medical therapies. “It is unavoidably in our future,” he says, “and I believe that it will become one of the central foci of our social debates later in this century and in the century beyond.” He warns that this might be accompanied by “serious errors and health problems as unknown genetic side effects in ‘edited’ children and populations begin to manifest themselves”.
For now, though, if there’s going to be anything even vaguely resembling the popular designer-baby fantasy, Greely says it will come from embryo selection, not genetic manipulation. Embryos produced by IVF will be genetically screened – parts or all of their DNA will be read to deduce which gene variants they carry – and the prospective parents will be able to choose which embryos to implant in the hope of achieving a pregnancy. Greely foresees that new methods of harvesting or producing human eggs, along with advances in preimplantation genetic diagnosis (PGD) of IVF embryos, will make selection much more viable and appealing, and thus more common, in 20 years’ time.
PGD is already used by couples who know that they carry genes for specific inherited diseases so that they can identify embryos that do not have those genes. The testing, generally on three- to five-day-old embryos, is conducted in around 5% of IVF cycles in the US. In the UK it is performed under licence from the HFEA, which permits screening for around 250 diseases including thalassemia, early-onset Alzheimer’s and cystic fibrosis.
As a way of “designing” your baby, PGD is currently unattractive. “Egg harvesting is unpleasant and risky and doesn’t give you that many eggs,” says Greely, and the success rate for implanted embryos is still typically about one in three. But that will change, he says, thanks to developments that will make human eggs much more abundant and conveniently available, coupled to the possibility of screening their genomes quickly and cheaply.

Advances in methods for reading the genetic code recorded in our chromosomes are going to make it a routine possibility for every one of us – certainly, every newborn child – to have our genes sequenced. “In the next 10 years or so, the chances are that many people in rich countries will have large chunks of their genetic information in their electronic medical records,” says Greely.
But using genetic data to predict what kind of person an embryo would become is far more complicated than is often implied. Seeking to justify unquestionably important research on the genetic basis of human health, researchers haven’t done much to dispel simplistic ideas about how genes make us. Talk of “IQ genes”, “gay genes” and “musical genes” has led to a widespread perception that there is a straightforward one-to-one relationship between our genes and our traits. In general, it’s anything but.
There are thousands of mostly rare and nasty genetic diseases that can be pinpointed to a specific gene mutation. Most more common diseases or medical predispositions – for example, diabetes, heart disease or certain types of cancer – are linked to several or even many genes, can’t be predicted with any certainty, and depend also on environmental factors such as diet.
When it comes to more complex things like personality and intelligence, we know very little. Even if they are strongly inheritable – it’s estimated that up to 80% of intelligence, as measured by IQ, is inherited – we don’t know much at all about which genes are involved, and not for want of looking.
At best, Greely says, PGD might tell a prospective parent things like “there’s a 60% chance of this child getting in the top half at school, or a 13% chance of being in the top 10%”. That’s not much use.
We might do better for “cosmetic” traits such as hair or eye colour. Even these “turn out to be more complicated than a lot of people thought,” Greely says, but as the number of people whose genomes have been sequenced increases, the predictive ability will improve substantially.
Ewan Birney, director of the European Bioinformatics Institute near Cambridge, points out that, even if other countries don’t choose to constrain and regulate PGD in the way the HFEA does in the UK, it will be very far from a crystal ball.
Nearly anything you can measure for humans, he says, can be studied through genetics, and analysing the statistics for huge numbers of people often reveals some genetic component. But that information “is not very predictive on an individual basis,” says Birney. “I’ve had my genome sequenced on the cheap, and it doesn’t tell me very much. We’ve got to get away from the idea that your DNA is your destiny.”
If the genetic basis of attributes like intelligence and musicality is too thinly spread and unclear to make selection practical, then tweaking by genetic manipulation certainly seems off the menu too. “I don’t think we are going to see superman or a split in the species any time soon,” says Greely, “because we just don’t know enough and are unlikely to for a long time – or maybe for ever.”
If this is all “designer babies” could mean even in principle – freedom from some specific but rare diseases, knowledge of rather trivial aspects of appearance, but only vague, probabilistic information about more general traits like health, attractiveness and intelligence – will people go for it in large enough numbers to sustain an industry?
Greely suspects, even if it is used at first only to avoid serious genetic diseases, we need to start thinking hard about the options we might be faced with. “Choices will be made,” he says, “and if informed people do not participate in making those choices, ignorant people will make them.”
Green thinks that technological advances could make “design” increasingly versatile. In the next 40-50 years, he says, “we’ll start seeing the use of gene editing and reproductive technologies for enhancement: blond hair and blue eyes, improved athletic abilities, enhanced reading skills or numeracy, and so on.”
He’s less optimistic about the consequences, saying that we will then see social tensions “as the well-to-do exploit technologies that make them even better off”, increasing the relatively worsened health status of the world’s poor. As Greely points out, a perfectly feasible 10-20% improvement in health via PGD, added to the comparable advantage that wealth already brings, could lead to a widening of the health gap between rich and poor, both within a society and between nations.
Others doubt that there will be any great demand for embryo selection, especially if genetic forecasts remain sketchy about the most desirable traits. “Where there is a serious problem, such as a deadly condition, or an existing obstacle, such as infertility, I would not be surprised to see people take advantage of technologies such as embryo selection,” says law professor and bioethicist R Alta Charo of the University of Wisconsin. “But we already have evidence that people do not flock to technologies when they can conceive without assistance.”
The poor take-up of sperm banks offering “superior” sperm, she says, already shows that. For most women, “the emotional significance of reproduction outweighs any notion of ‘optimisation’”. Charo feels that “our ability to love one another with all our imperfections and foibles outweighs any notion of ‘improving’ our children through genetics”.
All the same, societies are going to face tough choices about how to regulate an industry that offers PGD with an ever-widening scope. “Technologies are very amoral,” says Birney. “Societies have to decide how to use them” – and different societies will make different choices.
One of the easiest things to screen for is sex. Gender-specific abortion is formally forbidden in most countries, although it still happens in places such as China and India where there has been a strong cultural preference for boys. But prohibiting selection by gender is another matter. How could it even be implemented and policed? By creating some kind of quota system?
And what would selection against genetic disabilities do to those people who have them? “They have a lot to be worried about here,” says Greely. “In terms of whether society thinks I should have been born, but also in terms of how much medical research there is into diseases, how well understood it is for practitioners and how much social support there is.”
Once selection beyond avoidance of genetic disease becomes an option – and it does seem likely – the ethical and legal aspects are a minefield. When is it proper for governments to coerce people into, or prohibit them from, particular choices, such as not selecting for a disability? How can one balance individual freedoms and social consequences?
“The most important consideration for me,” says Charo, “is to be clear about the distinct roles of personal morality, by which individuals decide whether to seek out technological assistance, versus the role of government, which can prohibit, regulate or promote technology.”
She adds: “Too often we discuss these technologies as if personal morality or particular religious views are a sufficient basis for governmental action. But one must ground government action in a stronger set of concerns about promoting the wellbeing of all individuals while permitting the widest range of personal liberty of conscience and choice.”
“For better or worse, human beings will not forgo the opportunity to take their evolution into their own hands,” says Green. “Will that make our lives happier and better? I’m far from sure.”

Easy pickings: the future of designer babies
The simplest and surest way to “design” a baby is not to construct its genome by pick’n’mix gene editing but to produce a huge number of embryos and read their genomes to find the one that most closely matches your desires.
Two technological advances are needed for this to happen, says bioethicist Henry Greely of Stanford University in California. The production of embryos for IVF must become easier, more abundant and less unpleasant. And gene sequencing must be fast and cheap enough to reveal the traits an embryo will have. Put them together and you have “Easy PGD” (preimplantation genetic diagnosis): a cheap and painless way of generating large numbers of human embryos and then screening their entire genomes for desired characteristics.
“To get much broader use of PGD, you need a better way to get eggs,” Greely says. “The more eggs you can get, the more attractive PGD becomes.” One possibility is a one-off medical intervention that extracts a slice of a woman’s ovary and freezes it for future ripening and harvesting of eggs. It sounds drastic, but would not be much worse than current egg-extraction and embryo-implantation methods. And it could give access to thousands of eggs for future use.
An even more dramatic approach would be to grow eggs from stem cells – the cells from which all other tissue types can be derived. Some stem cells are present in umbilical blood, which could be harvested at a person’s birth and frozen for later use to grow organs – or eggs.
Even mature cells that have advanced beyond the stem-cell stage and become specific tissue types can be returned to a stem-cell-like state by treating them with biological molecules called growth factors. Last October, a team in Japan reported that they had made mouse eggs this way from skin cells, and fertilised them to create apparently healthy and fertile mouse pups.
Thanks to technological advances, the cost of human whole-genome sequencing has plummeted. In 2009 it cost around $50,000; today it is most like $1,500, which is why several private companies can now offer this service. In a few decades it could cost just a few dollars per genome. Then it becomes feasible to think of PGD for hundreds of embryos at a time.
“The science for safe and effective Easy PGD is likely to exist some time in the next 20 to 40 years,” says Greely. He thinks it will then become common for children to be conceived through IVF using selected genomes. He forecasts that this will lead to “the coming obsolescence of sex” for procreation.

Comments (…)
Sign in or create your Guardian account to join the discussion